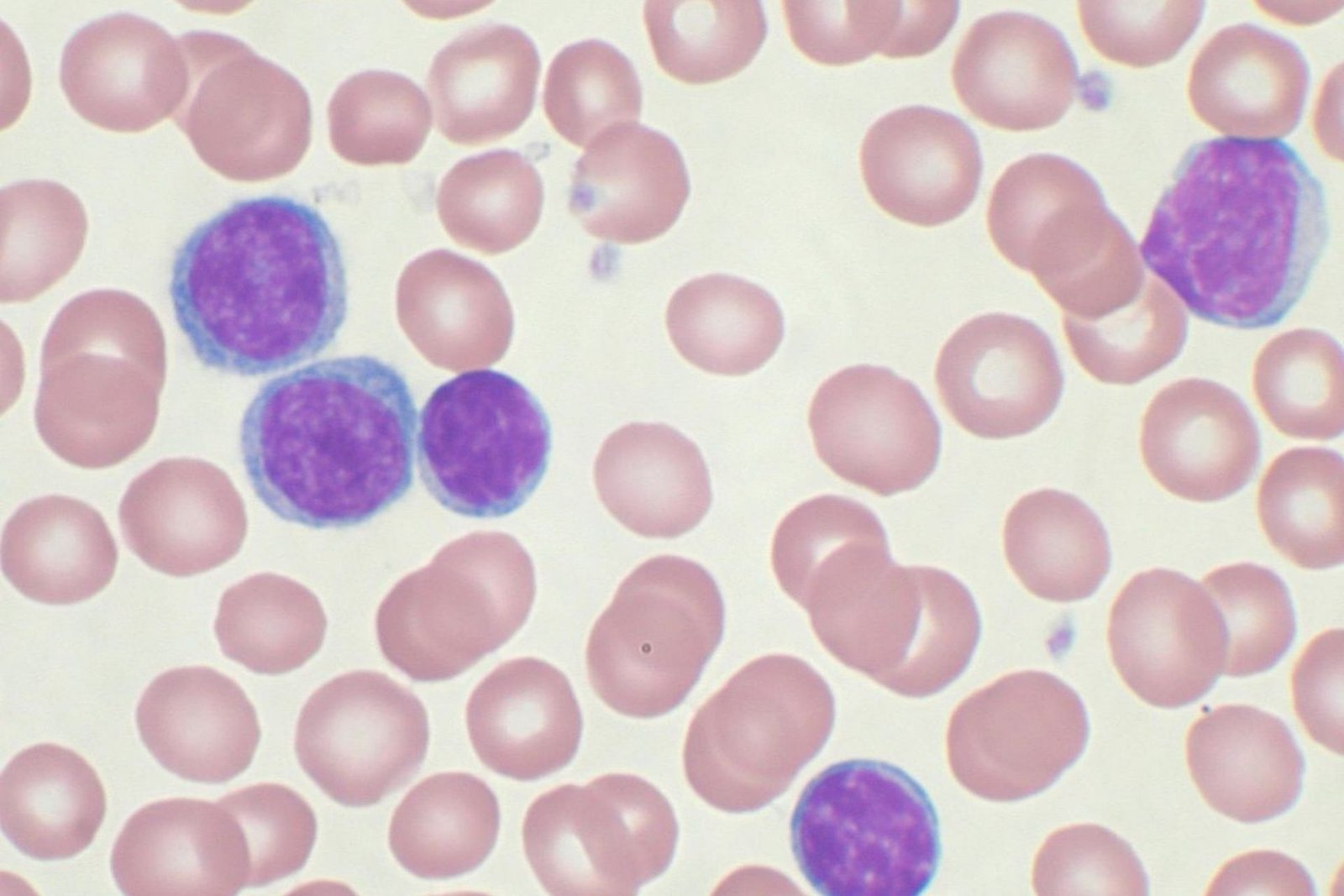
Brad S. Kahl, MD: The advancement of novel designated specialists in CLL [chronic lymphocytic leukemia] has changed this field. As anyone might expect, these new specialists have reliably performed better compared to conventional cytotoxic chemotherapy in stage 3 preliminaries.
As anyone might expect, when gatherings are beginning to dissect populace based information for long haul results, they’re seeing improvement in those results. We expect this is a direct result of the accessibility of these new specialists.
Ibrutinib has been around for a couple of years in CLL now and had adequate freedom to have an effect. Then, at that point we had venetoclax added to the alternatives and afterward acalabrutinib, and we’ve had the PI3 kinase inhibitors for various years—an entire host of new designated treatment choices in CLL.

There was an intriguing examination at ASCO [American Society of Clinical Oncology Annual Meeting] this year, where this gathering of agents took a gander at a SEER [Surveillance, Epidemiology, and End Results] data set investigation, and the time span they utilized was 1985 to 2017.
They had the option to show that the 5-year generally speaking endurance from the most punctual time stretch—they lumped it into 5-year time spans—worked on in men from 72% to 88%, contrasting the soonest time stretch with the most recent time span, and for ladies from 76% to 90%, from the most punctual time span to the most recent time span.
There it is clearly, solid proof that these new treatments are having a positive, advantageous impact on in general endurance in CLL. At the point when we’re surveying hazard in CLL, there are 2 primary boundaries to take a gander at.
There are some more recondite ones, yet those aren’t pretty much as key as these 2 primary ones. It’s really basic. It’s the immunoglobulin hefty chain quality mutational status, IGHV. This alludes to that CLL cell in its development, when it transformed into a threatening cell, or where that B cell can be considered as like the cell beginning: where the cell of beginning was the point at which it transformed into a CLL cell. Cells that have had dealing through the germinal focus of a lymph hub go through what’s called physical hypermutation.
That can be estimated, so for patients with CLL whose CLL cells are physically hypermutated, or something like that called IGHV changed, that ends up being ideal or acceptable in CLL. In the event that patients have the changed variant of IGHV, everything works better. Immunochemotherapy works better.
Venetoclax works better. With BTK [Bruton tyrosine kinase] inhibitors, it’s not really evident that those work better. They work similarly extraordinary in both changed and nonmutated, yet to have the transformed adaptation of IGHV is something beneficial for a patient. The other thing to take a gander at is the CLL FISH [fluorescence in situ hybridization] board. Assuming individuals have a 17p cancellation, that is a solid unfriendly prognostic marker.
These days it’s most likely worth sending the material for a TP53 change examination. Once in a while 17p and TP53 change go inseparably—travel together—however not generally.
That is a particularly significant unfavorable danger factor, that it merits knowing both 17p cancellation status and TP53 mutational status. Those are the 3 things I suggest. A CLL FISH board, TP53 mutational testing, and IGHV mutational testing.
Then, at that point you can have your patient danger defined enough. The IGHV-mutational status shouldn’t change after some time—you ought to need to do that test just a single time—however patients can procure a 17p erasure or a TP53 transformation over the long run. Before each time you start another line of treatment, it merits rehashing the FISH board and the TP53 mutational testing.
The standards for starting treatment doesn’t rely upon those danger factors we just referenced
All in all, in the event that you have a patient who has naturally high-hazard infection, since they’re IGHV unmutated, 17p erased, or TP53 transformed, that without anyone else isn’t motivation to begin treatment. The models for beginning treatment are the customary standards that have been distributed commonly.
Does the patient have manifestations? Assuming they have manifestations, beginning treatment is suitable. Is it accurate to say that they are turning out to be altogether pale? A hemoglobin level under 11 g/dL is a decent boundary.
Is it accurate to say that they are turning out to be essentially thrombocytopenic? A platelet check of 100,000 for every mm3 is a very decent boundary. Those are the most grounded rules. Somewhat gentler are things like the lymphocyte multiplying time. In the event that the lymphocytes twofold in 2 months, a few group say it’s an ideal opportunity to think about beginning treatment.
I don’t begin treatment dependent on the total lymphocyte tally; that is not a sign for treatment.

In some cases your patients are getting fundamentally cumbersome lymphadenopathy, and that would be motivation to begin, or indicative splenomegaly. They’re awkward from a major spleen. That is motivation to begin.
Cytopenias, essentially lymphadenopathy, critical splenomegaly, or the improvement of indications. Those are the fundamental motivations to start treatment in CLL.
_______________
Chronic | Don’t forget to follow us on Twitter @njtimesofficial. To get the latest updates